August 08, 2014
Despite Illinois’ tight budget for the current fiscal year, the State enacted major Medicaid legislation featuring increased payments to nursing homes and hospitals.
Public Act 98-0651 covers 231 pages and was the result of months of negotiations involving legislators, State officials and healthcare providers. The legislation was introduced as an amendment to an existing bill on May 26, 2014—the final week of the spring session. It cleared the House of Representatives on May 28, the Senate on May 29 and was signed into law on June 16.
In describing the new law, media reports, many lawmakers’ newsletters and a news release from Governor Pat Quinn’s office have focused on the additional benefits included for Medicaid recipients. A fact sheet describing the components of the legislation can be found on the website of the Illinois Department of Healthcare and Family Services (HFS), the State’s main Medicaid agency, but a breakdown of the costs has not been widely available.
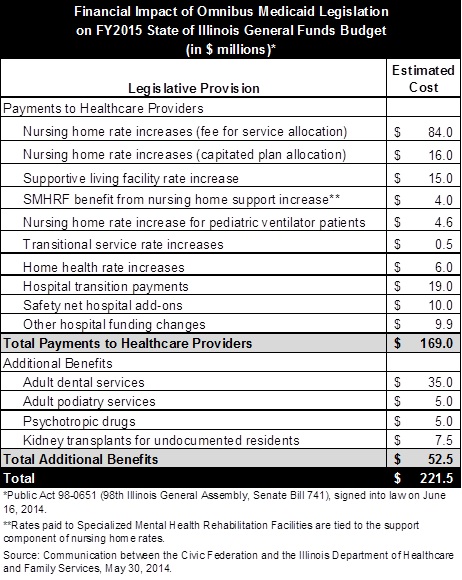
Data provided by HFS and shown in the following table indicate that the law is expected to cost the State’s general operating budget $221.5 million in FY2015. Of the total, additional payments to healthcare providers account for $169.0 million, or 76.3%, while additional medical benefits account for $52.5 million, or 23.7%. The HFS General Funds appropriation, which mainly covers Medicaid, is $7.3 billion in FY2015.
The added medical benefits mainly represent a restoration of benefits eliminated in 2012 under the Save Medicaid Access and Resources Together (SMART) Act. As discussed here, the SMART Act was designed to close a $2.7 billion gap in Medicaid funding by cutting costs and increasing revenues.
One of the most controversial cuts involved eliminating Medicaid coverage of adult dental services except for emergency care. Critics argued that the direct savings of $35.0 million would be wiped out by additional emergency room costs. Public Act 98-0651 brings back adult dental benefits that were provided before the SMART Act, which consisted of restorative services such as fillings and extractions but not preventive care such as cleanings. The restoration of this benefit had already been included in the Governor's FY2015 recommended budget. The new law also restores adult podiatry services and exempts psychotropic drugs from the limit of four prescriptions a month without prior authorization.
A new benefit under Public Act 98-0651, estimated to cost $7.5 million in FY2015, is kidney transplants for undocumented residents who are already receiving emergency renal dialysis services covered by Medicaid. Immigrants’ advocacy groups have recently urged that financial assistance be provided to undocumented residents who need organ transplants. Medicaid generally does not cover the undocumented, except for emergency care, although Illinois pays for medical services for undocumented children. Like those medical services, the newly authorized kidney transplants will be paid for with only State money. Medicaid is jointly funded by the State and federal governments, with State spending currently reimbursed by the federal government at a matching rate of 50.0%. That means that for most of the costs shown in the table, the State’s net cost—after federal reimbursement—is half of the total amount.
The largest rate increases in Public Act 98-0651 are for nursing homes. In a publication for members, the Health Care Council of Illinois, a nursing home trade group, claimed a $100 million victory due to rate increases in the new law. Specialized Mental Health Rehabilitation Facilities (SMHRFs), which were formerly known as Institutions for Mental Diseases, benefit from the nursing home rate increase because their rates are linked to nursing home rates. State spending for SMHRFs is not reimbursed by the federal government.
The law also includes elements of a Nursing Home Residents' Managed Care Rights Act pushed by the Health Care Council. Some consumer advocates contended that the bill was designed to block HFS’ plans for managed care, specifically a demonstration project for recipients of both Medicare and Medicaid. Managed care organizations are paid a set monthly fee by the State for each member. Nursing homes might face empty beds if managed care organizations can move the elderly out of nursing homes and into community settings to save money and potentially improve care. Although parts of the nursing home rights act were included in Public Act 98-0651, the demonstration project is scheduled to proceed for nursing home residents after several delays.
The new law authorizes projected General Funds payments of $38.9 million to hospitals in FY2015. Of that amount, $19 million is a transition payment designed to prevent hospitals from suffering financially from a new rate-setting methodology that took effect on July 1. The HFS budget for FY2015 previously included $70 million for such transition payments, and total transition payments to hospitals through FY2017 amount to $290 million. The FY2015 budget also includes $130 million to alleviate losses to nursing homes due to a new rate system for those facilities.
Other significant provisions of Public Act 98-0651 do not affect the FY2015 general operating budget. The new law extends through FY2017 two hospital assessment programs that were due to expire at the end of calendar year 2014. A hospital assessment program is a Medicaid funding device that uses payments from hospitals to draw additional federal funds that are mainly paid back to hospitals. The law also provides that HFS will seek federal approval to receive roughly $400 million more in federal matching funds from the assessment programs based on the 100% matching rate available for newly eligible Medicaid recipients through calendar year 2016 under the Affordable Care Act (ACA).
Public Act 98-0651 authorizes Cook County’s public health system to be licensed as a health maintenance organization, which will allow it to enroll individuals who are not eligible for Medicaid in its health plan. As discussed here, the Cook County Health and Hospitals System’s CountyCare started as a plan for newly eligible Medicaid enrollees under the ACA and is expanding to cover other Medicaid patients. The Health System plans to form a licensed HMO to include participants in the new ACA insurance exchange.
Other provisions of the new law are designed to help expedite the processing of Medicaid applications for nursing home residents. The Health Care Council had argued that the backlog of applications violated federal processing guidelines. Under the law, nursing homes with significant costs due to residents whose Medicaid applications are pending can receive up to a total of $50 million in loans, which must be repaid by the end of FY2015.